Reviewed by Dr. Dustin B. Rinehart
TLDR: Cold weather often brings increased joint pain due to changes in temperature and pressure. When temperatures drop, arthritic joints may become stiff, swollen, and irritated. Cooler air, lower barometric pressure, and reduced physical activity can trigger discomfort. Early supportive care with dedicated exercises, over the counter medication, and support from an orthopedic specialist can ensure colder months remain tolerable. If you want help easing seasonal joint pain, TSAOG offers both physical therapy for arthritis and advanced joint preservation options that keep people moving comfortably year-round.
Why Cold Weather Can Make Joint Pain Worse
Many people notice their joint pain increases when a cold front rolls in. While the experience varies from person to person, weather changes may affect the tissues around your joints. Colder temperatures can make muscles and connective tissues tighten, which reduces flexibility and increases the feeling of stiffness. That small change can lead to increase pain in already sensitive joints.
Barometric pressure also plays a role, similar to temperature, in that it may impact tissues around your joints. This small shift often increases soreness, especially for those with inflammation-based conditions like arthritis. You may feel the effects most in weight-bearing joints such as knees, hips, and ankles, but hands and fingers can react strongly as well.
Reduced movement during winter adds another layer. People naturally move less when it’s cold, which means joints don’t get the usual workout they need to remain limber. Without regular movement, stiffness becomes more noticeable, and pain builds quickly.
How Arthritis Reacts to Seasonal Changes
Arthritis already involves inflammation, so the different weather can intensify symptoms. If your arthritis symptoms normally fluctuate, seasonal shifts may make those changes more pronounced.
Osteoarthritis often feels worse in winter because the joint is no longer warm and flexible. Meanwhile, inflammatory conditions like rheumatoid arthritis or psoriatic arthritis may flare when weather changes.
It’s also worth remembering that colder weather often changes daily routines. People may skip outdoor walks or stay indoors longer. Without steady movement, joints become less resilient. Even a few days of inactivity can create a noticeable increase in symptoms for those living with arthritis.
The good news is that managing these changes is possible with a combination of self-care, consistent activity, and support from a specialist when you need it.
Tips to Manage Joint Pain in Cold Weather
Stay Warm and Layered
Keeping your joints warm helps them stay flexible and less reactive to temperature swings. Light layers, gloves, warm socks, and heated blankets can make day-to-day movement feel easier.
Keep Moving, Even in Small Ways
Gentle, regular activity keeps circulation steady and reduces the feeling of stiffness in cold weather. Indoor stretching routines, low-impact cardio, or short strength sessions can all keep joints more comfortable. Even a few minutes of walking around the house or doing mobility exercises during breaks can make a difference when it’s too chilly to be outside for long.
Try Warm Showers or Heat Packs
Heat encourages tight tissues to relax and move more easily. A warm shower in the morning can loosen up stiff joints, while a heating pad in the evening helps calm lingering soreness.
Support Joints During Activity
Braces, supportive footwear, and cushioned insoles can reduce stress on sensitive joints and make daily activities more manageable. These small adjustments help you stay active without adding unnecessary strain, especially when sidewalks are uneven, slippery, or cold enough to make muscles tense.
Stay Hydrated and Eat Warm Meals
Hydration keeps joint tissues healthier and more resilient. Warm foods like soups, stews, and herbal teas offer comfort while also helping you meet your fluid needs during a season when people tend to drink less water.
Maintain a Consistent Routine
Joints often tolerate weather changes better when you maintain steady habits. Regular movement, predictable sleep patterns, and consistent activity levels help regulate inflammation and prevent big swings in stiffness or pain.
When to See an Orthopedic Specialist
If your joint pain becomes hard to manage, limits daily activities, or flares up every winter without much relief, a specialist can help you create a plan that aligns with your health, age, and activity level.
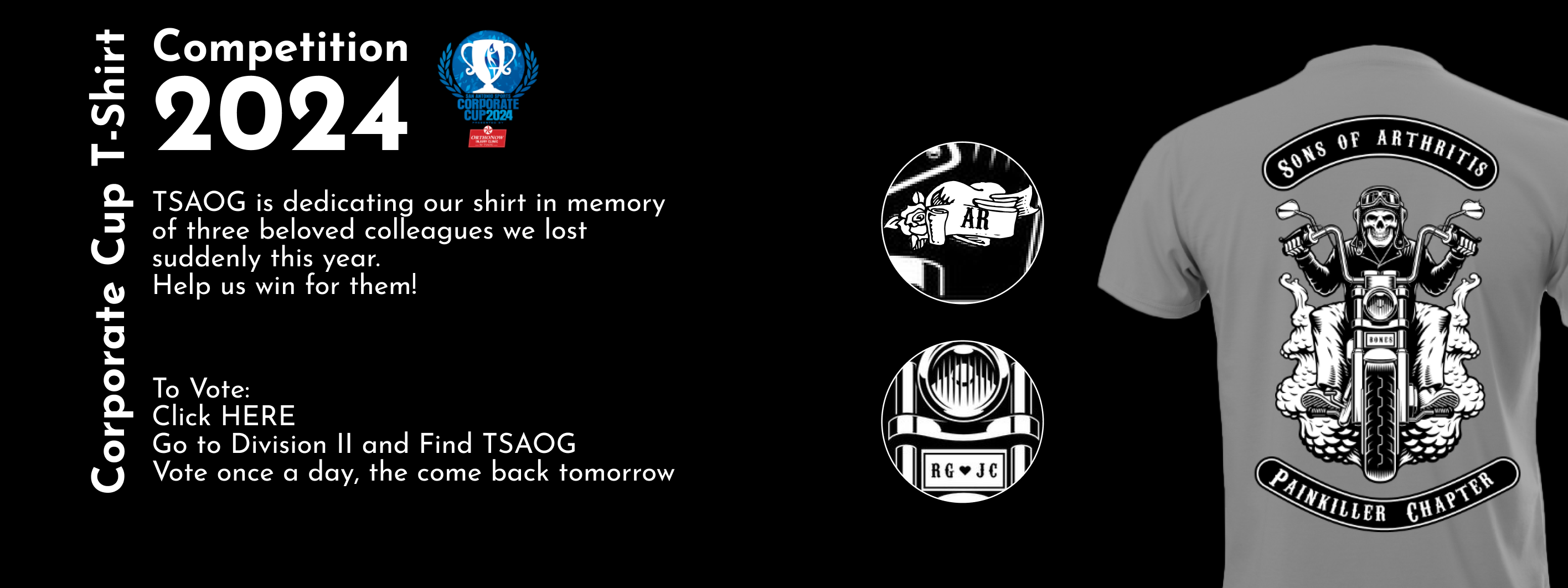
TSAOG helps patients manage arthritis pain year-round by focusing on your individual symptoms, lifestyle, and long-term goals. Their team supports patients through every stage of arthritis care, offering detailed evaluations, personalized treatment plans, and long-term guidance that adapts as your needs change. With a full range of specialists, diagnostic tools, and both conservative and advanced treatment options, TSAOG provides the clarity and support you need to stay active in any season.
If colder weather is making your joints ache more than usual, you don’t have to suffer. Talking with a TSAOG provider can help you figure out what’s driving your symptoms and discuss options for improvement.
Resource:
https://www.uhhospitals.org/blog/articles/2024/01/is-joint-pain-worse-in-cold-weather