Podiatry Center
What Is A Podiatrist?
A podiatrist, or doctor of podiatric medicine (D.P.M.), is a specialist in the medical and surgical care of conditions of the foot. At TSAOG Orthopaedics & Spine, our podiatrists are board certified in their fields and have all gone through 4 years of podiatric medical school and 3 years of residency training.
Dr. David Hughes is a podiatrist, board-certified in foot surgery by the American Board of Podiatric Surgery, which has been recently renamed the American Board of Foot and Ankle Surgery (ABFAS).
Dr. Jessica Rutstein is a podiatrist, board-certified in primary care in podiatric medicine by the American Board of Multiple Specialties in Podiatry (ABMSP).
Conditions Treated:
- Arch Disorders
- Arch Pain
- Arthritis of the Foot
- Athlete’s Foot
- Blisters
- Bone Pain
- Bone Spurs
- Bunions
- Burning Feet
- Bursitis
- Calluses
- Capsulitis
- Charcot Foot
- Chilblains
- Claw Toe
- Corns
- Cysts
- Diabetic Ulcers
- Digital Deformity
- Dry Skin
- Edema
- Enchondroma
- Flat Feet
- Foot Deformity (Pediatric)
- Foot Fractures
- Foot Fungus
- Foot Infections
- Foot Odor
- Freiberg’s Disease
- Frostbite
- Ganglion Cysts
- Gangrene
- Gout
- Hallux Limitus
- Hallux Rigidus
- Hallux Varus
- Hammertoe
- Heel Callus
- Heel Fissures
- Heel Pain
- Ingrown Toenails
- Intoeing and Outtoeing
- Ischemic Foot
- Kohler’s Disease
- Mallet Toes
- Metatarsalgia
- Neuritis, Nerve Pain
- Neuromas
- Osteochondromas
- Osteomyelitis
- Overlapping and Underlapping Toes
- Peripheral Neuropathy
- Plantar Fasciitis
- Plantar Fibromas
- Posterior Tibial Tendon Dysfunction
- Psoriasis
- Raynaud’s Disease
- Sesamoiditis
- Severs Disease
- Skin Allergies
- Skin Lesions
- Spasms
- Sports Injuries of the Foot
- Stress Fractures of the Foot
- Subungal Exostosis
- Tendinitis
- Tendon and Joint Pain
- Tinea Pedis
- Toenails
- Turf Toe
- Ulcers
- Venous Stasis
- Warts
Procedures Offered:
- Bunionectomy / Bunion Surgery
- Custom Made Orthotics
- Cryoprobe for Plantars Warts
- Foot Spur Removal
- Foreign Body Removal
- Ganglion Cyst Treatment
- Hallux Rigidus / Limitus Surgery
- Hammertoe Surgery
- Heel Pain Treatment – Conservative and Surgical
- Ingrown Toenail Removal
- Metatarsal Surgery
- Nerve Surgery for Neuroma
- Orthotics
- Routine Foot Care
- Toenail Problems
- TOPAZ for Plantar Fasciitis
- Wart Treatment
Your Podiatry Team
Book an Appointment
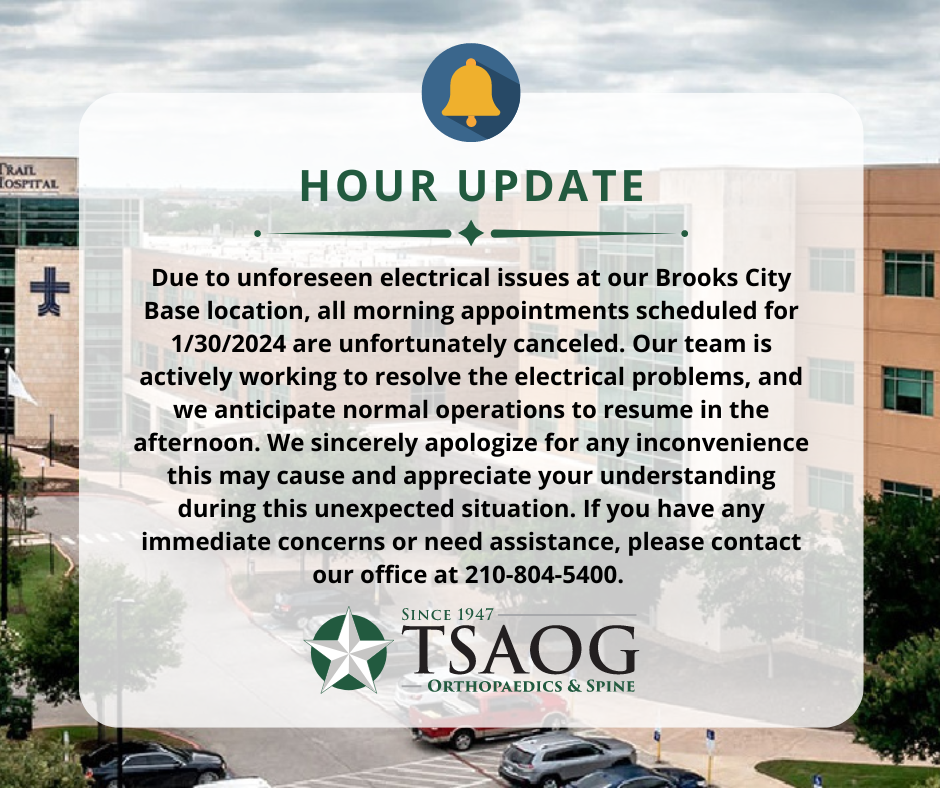
FIND A LOCATION

Christus Santa Rosa NW, Tower I
2829 Babcock Rd., #700
San Antonio, TX 78229










Ridgewood Orthopaedic Center
19138 US-281 N
San Antonio, TX 78258
PHYSICIANS: Jeffrey B. Shroff, M.D. , Alexander S. Rowland, M.D. , Stephen C. Drukker, M.D. , Taneka M. Stewart, DNP, FNP-BC , Linzy Fitzsimons, M.D. , Jonathan S. Duncan, M.D. , Jessica F. Rutstein, D.P.M. , David E. Vizurraga, M.D. , M. Brandon Dobson, M.D. , Lauren E. Karbach, M.D. , Michaelia Sunderland, M.D. , G. Lane Naugher, M.D. , Justin Robbins, M.D. , Joseph Poku, M.D. , Eloy Ochoa, Jr., M.D. , S. Josh Bell, M.D. , Bryan W. Kaiser, M.D. , Richard L. Ursone, M.D. , Matthew C. Swann, M.D. , Sergio Viroslav, M.D. , Randall C. Marx, M.D. , David R. Espinoza, M.D. , Casey D. Taber, M.D. , Scott R. Seidel, D.C. , Ronald W. Connor, M.D. , Dustin B. Rinehart, M.D. , Frank J. Garcia, M.D. , B. Christian Balldin, M.D. , Ephraim K. Brenman, D.O., R.M.S.K. , Robert U. Hartzler, M.D., M.S. , David T. Hughes, D.P.M.










Westover Hills Medical Plaza I
11212 State Hwy 151, #150
San Antonio, TX 78251
PHYSICIANS: Jonathan S. Duncan, M.D. , Nicholas Nira, D.C. , S. Josh Bell, M.D. , Emmanuel C. Nwelue, Jr., M.D. , Shane C. Eizember, M.D. , G. Lane Naugher, M.D. , Eloy Ochoa, Jr., M.D. , Kevin L. Kirk, D.O., F.A.O.A. , Christian A. Woodbury, M.D. , Stephen T. Gates, M.D. , Casey D. Taber, M.D. , Anthony Montanez, M.D.
Ridgewood Orthopaedic Center
Ridgewood Orthopaedic Center
19138 US-281 N.
San Antonio, TX 78258
Medical Center
Christus Santa Rosa NW, Tower I
2829 Babcock Rd., #700
San Antonio, TX 78229
Westover Hills
Westover Hills Medical Plaza I
11212 State Hwy 151, #150
San Antonio, TX 78251